Cartilage degeneration is a common disease of the intervertebral disc, occurring in people of many different ages.Today, it is diagnosed in more than 40% of fairly young people under 35 years of age, and among older people, it affects 9 out of 10 people.It has many stages of development, and the earlier the pathology is detected, the easier and more effective the treatment and the lower the risk of developing dangerous complications.
What is osteoarthritis?
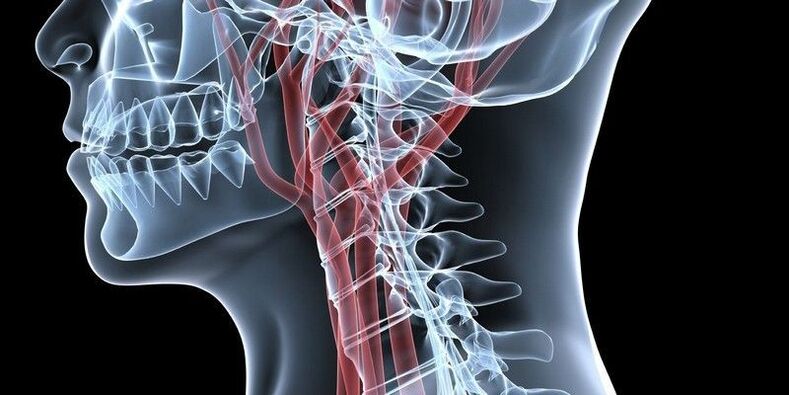
The intervertebral disc is located between the vertebral bodies and is a type of shock absorber that helps absorb stress when walking or performing other physical activities.They vary in size depending on their location: in the cervical region, the intervertebral discs are the smallest, and in the lumbar spine, they are the largest.
All are built the same.In the center is the nucleus pulposus, which is the main component of the intervertebral disc and has high elasticity.It is surrounded by a fibrous membrane and end plates.
Chondrolysis is a degenerative-dystrophic disease, in which there is a change in the shape and size of the intervertebral discs due to their wear and creates prerequisites for the formation of hernias, deformation of the vertebral bodies, spondylosis and other disorders.
Thinning of the intervertebral disc is a consequence of malnutrition of the cartilage tissue, leading to a gradual decrease in elasticity and increased brittleness.
As a result, the intervertebral discs change position, their height decreases, and small cracks form in their fibrous membranes.This creates a serious premise for the formation of intervertebral hernia, compression of spinal roots or blood vessels.
The slightest changes in the condition of the discs will lead to disruption of their function.This is accompanied by pain of varying degrees.At the same time, it creates prerequisites for the development of diseases of internal organs, since the quality of their functioning directly depends on the condition of the spine and the conductivity of bioelectric impulses along the nerves.
It can affect one or more discs in any part of the spine.Therefore, osteoarthritis is diagnosed:
- cervical spine;
- thoracic spine;
- lumbar spine.
In especially severe cases, the pathological process involves most of the intervertebral discs of the spine, accompanied by discomfort throughout the back and almost complete loss of ability to function.But most often, osteoarthritis affects the lumbar spine, since it bears the greatest load, as well as the intervertebral discs of the cervical spine due to their high mobility.
Develop
In the process of osteoarthritis, 4 stages can be roughly distinguished:
- The hydration level of the disc decreases, leading to dehydration and the formation of microcracks.Often at this stage there are still no signs of the disease in its early stages.
- The height of the intervertebral disc decreases, leading to the appearance of the first pathological symptoms.At this stage, the distance between individual segments decreases, which leads to a decrease in the tone of the spinal ligaments and creates the possibility of the vertebrae being displaced from their natural position, that is, the development of spondylolisthesis.In such situations, a wave-like disease progression is most often observed.It can distinguish between periods of exacerbation, accompanied by acute pain, and periods of remission, in which there is no discomfort at all or pain.
- Deformation of the affected intervertebral disc with protrusion or prolapse formation.Sometimes there is involvement of the joints in the pathological process, manifested by the development of arthropathy or subluxation of the vertebrae.At this stage, the immune system reacts to the processes occurring in the spine by developing sterile inflammation accompanied by swelling of the tissues surrounding the affected spinal motor segment.In this case, pain occurs frequently, reflex muscle spasms as well as limitation of movement can be observed.In rare cases, signs of neurological deterioration (nerve root syndrome) have developed due to compression of nerve fibers by a protruding disc.
- Development of complications.Because the human body has extensive compensation capabilities, when the intervertebral disc loses the ability to perform its functions, osteosynthesis is activated to fix the vertebrae in a stable position.This leads to the formation of bony projections - osteophytes - at the edges of the vertebral bodies of the affected spinal motion segment.As a result, thanks to them, two or more vertebrae fuse tightly together, forming a single conglomerate, that is, spondylosis develops.This always leads to compression of the nerve and the development of acute neurological symptoms in the form of paralysis, paralysis and serious disorders in the functioning of the corresponding internal organs.
Reason
Today, there are many theories about the development of osteoarthritis, including vascular, mechanical, genetic, hormonal, infectious-allergic and others.But none of them can fully explain the mechanism of development of changes in the tissue of the intervertebral disc.So, most likely, they all complement each other.
Therefore, a large number of very diverse factors can lead to the development of osteoarthritis.Among them, the most significant are:
- genetic predisposition;
- regularly perform heavy work;
- maintain a sedentary lifestyle;
- presence of scoliosis or other spinal deformities;
- back injury;
- unbalanced diet, lack of vitamins;
- infectious diseases;
- metabolic disorders;
- congenital malformations of the spine (Kimerli malformation, Chiari malformation, craniofacial malformation, sacralization, lumbar);
- overweight;
- Frequent severe stress.
It is believed that the most significant influence on the condition of the intervertebral discs is the constant overload of a certain segment of spinal movement.This can be due not only to performing monotonous heavy physical work, but also to constant hunching or the habit of sitting for long periods of time.In such situations, additional stress is placed on the discs, muscles and ligaments and other factors that only aggravate the situation.
In general, osteoarthritis can be called an almost natural age-related disease, which is the inevitable price of going straight.
Symptom
The earliest sign of the development of the disease is the appearance of crunching sounds in the spine, where degenerative-dystrophic changes begin.It is a consequence of the appearance of nutritional disorders of the intervertebral disc and the progression of dehydration.At this stage, patients almost never seek medical help.Therefore, their daily living habits, eating habits and other factors remain the same, which contributes to the situation becoming worse and the disease progressing to stage two.
As a result, typical symptoms of osteoarthritis begin to appear:
- severe muscle tension in the affected area on only one or both sides of the spine;
- sharp and aching pains, increasing with each movement and increasing with time, became unbearable;
- numbness in the arms or legs;
- weakness;
- stiffness of movement, restriction of unauthorized movement;
- decreased muscle tone to complete muscle atrophy;
- bad posture;
- high blood pressure.
As the disease progresses, signs of osteoarthritis become more severe.80% of patients feel a dull pain in the affected area of spinal movement, which is also characteristic of myositis.
Cervical spine degeneration
When the cervical spine is affected, pain tends to spread to the shoulder blades, arms and other neurological disorders appear.The patient keeps the head in the least painful position and, if necessary, turns the whole body.
In addition, pathologies of organs innervated by the spinal cord region of the cervical spine may develop:
- tinnitus and diseases of the ENT organs;
- dizzy;
- blurred vision;
- migraine headache;
- Increased levels of irritability and anxiety;
- sleep problems;
- increased risk of allergic reactions;
- reduced thyroid hormone levels.
With cervical spondylosis, vertebral artery syndrome and vegetative-vascular dystonia are often additional diagnoses.
Infection of the cervical spine with osteonecrosis, especially when complicated by intervertebral protrusion and herniation, can lead to compression of blood vessels.This leads to impaired blood supply to the brain, which can be accompanied by dizziness, loss of consciousness and even stroke.
Osteoarthritis of the thoracic spine
With osteoarthritis of the thoracic region, which is diagnosed quite rarely, pain occurs in the spine at the level of the shoulder blades and can intensify even with deep breathing.They are often felt behind the sternum and can be confused with heart disease.
When the spinal roots are compressed, the risk of internal organ diseases increases, specifically:
- bronchial and pulmonary (asthma, bronchitis, pneumonia, pleurisy);
- gallbladder and bile ducts, liver (cholecystitis, jaundice, fat absorption disorders);
- pancreas and duodenum (digestive disorders, left upper quadrant pain);
- adrenal glands, which affect the overall strength of the immune system and can stimulate the development of allergies;
- kidney (urinary disorders, chronic pyelonephritis, glomerulonephritis, etc.);
- Pelvic organs (digestive disorders, gynecological and urinary diseases, infertility).
Fact: damage to the intervertebral disc of the 7th thoracic vertebra due to osteoarthritis can lead to the development of diabetes.
Osteoarthritis of the lumbosacral spine
With osteoarthritis in the lumbar region, lumbar pain is observed, which is called lumbar pain.Accompanied by a burning, uncomfortable feeling that occurs suddenly.Often, patients even find it difficult to sit down, get up and walk, which may indicate the development of nerve root syndrome.In such situations, it is easy to see them slowly sitting down and standing up, trying to avoid tilting their torso as much as possible.
If complications occur, the main danger is compression of the nerves of the cauda equina, as this can lead to impaired control of bowel and bladder emptying, as well as paralysis of the legs.In addition, in such cases, the following may develop:
- appendicitis;
- diarrhea, constipation;
- lower abdominal pain;
- bladder dysfunction;
- impotent;
- pain in the knees, feet, hips, or groin area;
- leg swelling.
complications
Osteonecrosis is a possible cause of a large number of different diseases.Usually, if left untreated, it leads to the formation of protrusions and herniations between the vertebrae.This in turn can cause:
- myelopathy due to intervertebral disc, leading to paralysis, muscle atrophy, changes in tendon reflexes, loss of control over urination and defecation, and even paralysis of the limbs;
- radiculopathy;
- scoliosis or other spinal deformity;
- Spinal cord infarction due to compression of the artery that feeds it;
- stroke due to compression of the occipital artery.
Diagnose
The appearance of pain in the back and neck should be a reason to contact a neurologist or vertebra specialist.The earlier osteoarthritis is diagnosed, the easier and more effective treatment will be.
To diagnose the disease, the doctor interviews and examines the patient.Based on their results, the presence of degenerative changes in the intervertebral discs can be assumed.But for final diagnosis, instrumental diagnostic methods are prescribed, which include:
- MRI;
- CT;
- x-ray in two projections.
Magnetic resonance imaging provides the most complete information about the condition of the intervertebral disc.This procedure is mainly performed in closed-type devices with a capacity of 1.5 T. With its help, you can distinguish osteoarthritis from tuberculous spondylitis, osteomyelitis, infectious diseases, etc.
CT scans and X-rays provide information about the bony structure of the spine.Thanks to them, one can detect displacement of the vertebral bodies, the presence of bone spurs and other disorders.
Additionally, the following may be prescribed:
- Ultrasound Dopplerography of cervical vessels;
- electromechanics;
- research in the laboratory.
Treatment of osteoarthritis
Therapy is developed individually for each patient.In this case, the severity of the degenerative-dystrophic process, the presence of complications, the nature of the patient's work activity and a variety of other factors must be taken into account.
All patients must be prescribed a series of measures, since it is impossible to eliminate pathological changes in the intervertebral disc only with the help of drugs.Components of conservative therapy for osteonecrosis may include:
- drug treatment;
- osteopathy;
- manual therapy;
- physical therapy (phonotherapy, ozone therapy, carboxytherapy, pressure therapy, RF current);
- Personal training sessions with a rehabilitator.
All patients diagnosed with disc dystrophy should reconsider their lifestyle.It is necessary to make time for moderate physical activity, especially for people in sedentary occupations, or conversely, think about the possibility of changing careers for those who are forced to lift heavy objects every day.
But in the acute stage, complete rest is recommended.It is ensured not only by maintaining bed rest, but also by wearing an orthopedic bandage: in case of damage to the cervical spine, use a Shants collar;In case of osteoarthritis of the lumbar region, a corset should be worn.

In the first stages of the development of the disease, it is usually enough to adjust your lifestyle, engage in exercise therapy and visit a chiropractor.In more severe cases, medical treatment and physical therapy are necessarily prescribed.
Never resort to self-medication by dubious means, self-prescribing anti-inflammatory drugs, as well as dubious "healers" who position themselves on the Internet: you can lose not only your time and money, but also your health.
Treatment with medication
For osteoarthritis, a complex of drugs is prescribed to relieve pain, eliminate inflammation and reflex muscle spasms, improve nerve conduction and activate tissue regeneration of the intervertebral disc.
So, the patient is prescribed:
- NSAIDs – help relieve pain and have anti-inflammatory effects;
- corticosteroids – exhibit powerful anti-inflammatory properties;
- muscle relaxants – eliminate muscle spasms, help relieve back pain;
- Vitamin B – helps improve the function of the nervous system in general and the transmission of nerve impulses along each nerve in particular;
- vitamin D is a remedy responsible for the condition of bone tissue, as well as higher functions of the brain, such as memory, attention, speech;
- chondroprotectors – nourish the intervertebral discs with compounds necessary for the construction of new fibers of the nucleus pulposus;
- Psychotropic drugs – increases the effectiveness of non-steroidal anti-inflammatory drugs and muscle relaxants;
- Vascular medicine - improves blood circulation in the tissues surrounding the spine, ensuring a more active supply of nutrients and oxygen to the intervertebral discs;
- Anticonvulsants – used in rare cases to relieve very severe spasms.
For very severe pain, often presenting complications, the patient can apply back blockade, which provides immediate results.Sometimes corticosteroid hormones are added to the solution to effect a blockade.This also leads to a pronounced anti-inflammatory effect.
The blockade is carried out in absolutely sterile conditions, which can only be achieved in specialized medical facilities.At the same time, they require special knowledge and skills, so only highly qualified medical personnel can successfully complete the task.Otherwise, there is a high risk of infection or nerve fiber damage, leading to the development of serious complications.

During a block, injections are usually given on both sides of the spine in the area where the nerves causing pain are located.There are several techniques for performing them, of which the specific technique is selected individually by the doctor.
But blockades should be carried out no more than 4 times a year.Since with osteochondrosis, acute, painful attacks occur much more often, it is necessary first of all to direct efforts to eliminate the cause of their occurrence, that is, the degenerative-dystrophic process in the joint itself.
Manual therapy
Manual therapy sessions are indicated outside of the exacerbation of osteonecrosis.They play one of the leading roles in the treatment of the disease, since the competent use of manual techniques on the spine and surrounding tissues not only helps to stop the progression of pathological processes in intervertebral discs, but also creates the most favorable conditions for their recovery.
In addition, certain techniques can also have a positive effect on the functioning of internal organs.For example, one of the methods is designed, by normalizing the position of each vertebra, to remove pressure on the spinal roots, blood vessels and spinal membranes and thereby restore the normal connection of the organ with the nervous system.This helps eliminate the underlying causes that led to the development of the above diseases of the heart, bronchus, lungs, kidneys, gastrointestinal tract and reproductive system and leads to complete recovery.

Thanks to the precise impact of jewelry on the spine, not only blood circulation and acceleration of metabolism are activated, as with classical therapeutic massage, but also the launch of natural self-healing mechanisms.Eliminating scoliosis, incorrect vertebral position, and other pathological changes in the spine through manual therapy can further strengthen the immune system, improve overall health, and significantly improve quality of life.
Positive changes can be noticed after the first session, and in the future their severity will only increase.
Physical therapy
Physical therapy procedures increase the effectiveness of all other osteoarthritis treatments and help reduce pain.Most commonly used:
- electrophoresis - the use of electric current to ensure the penetration of anesthetics, anti-inflammatory drugs and other substances directly into the site of inflammation, allowing you to quickly achieve a noticeable therapeutic effect;
- Ultrasound therapy - the effect of ultrasound provides pain relief, increases the intensity of metabolic processes in the affected area and creates prerequisites for high-quality restoration of thinned intervertebral discs;
- decompression therapy – involves stretching and massaging the spine on a special ribbed mattress, which helps activate blood circulation and increase muscle tone;
- Traction therapy or spinal traction – is performed using special devices that create traction on the spine, due to which the distance between the vertebrae increases and the pressure on the worn disc decreases sharply, allowing it to recover more actively.

All procedures are prescribed in courses of 10–15 sessions.When choosing them, they take into account not only the condition of the intervertebral discs, but also the presence of accompanying diseases, since some of them have contraindications to certain physical effects.
Exercise therapy
Osteoarthritis therapeutic exercises play an important role, since correctly selected exercises for the treatment of damage to different parts of the spine can help form a strong muscle corset, while eliminating increased muscle tone.This will provide good support for the spine and prevent the progression of degenerative disc disease.In addition, exercise therapy helps activate blood circulation and increase the intensity of metabolic processes.
Building a physical therapy program is the responsibility of the rehabilitation physician.Based on the severity of spinal damage, the patient's physical development characteristics, age and other factors, the doctor will create an optimal set of exercises, the implementation of which will create optimal loads for the muscles and spine.
The first classes must be conducted under the supervision of a doctor.After the patient learns how to properly perform each exercise, he is allowed to continue practicing at home.It is important to avoid any sudden movements.All exercises are performed daily slowly and rhythmically, the load gradually increasing.But the appearance of pain during exercise is a good reason to refuse to perform the exercise that provoked it.

prevent
It is much easier to prevent the development of the disease than to deal with its consequences later.Since osteoarthritis can happen to everyone sooner or later, you should think about possible risks as early as possible and do your best to prevent this.Therefore, each person should adhere to the following recommendations:
- Avoid physical exertion, regular exercise, swimming, and when working sedentary, take regular breaks to warm up;
- Pay attention to your posture when walking or sitting;
- buy high quality orthopedic mattresses and pillows;
- Observe correct lifting technique: back straight and knees bent;
- replace casual shoes with the most comfortable ones and save dress shoes for special occasions;
- Eat properly so that your body does not suffer from nutritional deficiencies and your weight remains within normal limits.
There is only one way to avoid the appearance and manifestation of osteoarthritis symptoms - start taking care of yourself and your health.Since osteoarthritis is not just one disease, but a complex of muscle-tonic changes and neurodystrophy, which is the body's reaction to physical inactivity, chronic static tension of the spinal muscles, environmental conditions and chronic neurological disorders, especially common among city dwellers, swimming in the pool and stretching programs, including yoga.
So, osteoarthritis is a very common disease, but if you pay careful attention to your health, you can effectively fight it at any age.But ignoring the problem will not lead to anything good and sooner or later will force the patient to lie on the operating table.
























